There is a non-zero chance that I am becoming a diabetes tech nerd. The long-awaited iLet Bionic Pancreas is the insulin-only version of the dual-hormone insulin pump that is the holy grail of insulin deficient diabetes management. BetaBionics has been working on a dual hormone pump for over a decade. While the dual-hormone version of the iLet is in human trials, they opted to release the insulin-only version of the pump. When the iLet release was announced in May 2023, I shrugged and signed up to be notified when it was available, figuring I'd take the new and improved loop algorithm for a test spin (especially since it has it's origins in the DIY looping community). I've had extremely good success with Tandem's Control IQ (CIQ) algorithm, but was micromanaging and manipulating the system by taking several insulin doses over the course and after a meal as the food absorbed, and taking occasional small manual boluses to bump my blood glucose (bg) into my target range. Ultimately, I've been administering insulin in a way that vaguely reflects the super micro boluses (SMBs) utilized by the iLet and several DIY loop algorithms. So in an attempt to relieve some of the mental burden of actively managing my diabetes, I got my hands on an iLet and took it for a spin.
At the time of writing, the iLet is compatible with the Dexcom G6 continuous glucose monitor (CGM), with a software update for the Dexcom G7 and Abbot's Libre 2 forthcoming (update: G7 approval in US in Dec. 2023). Similar to other insulin pumps on the market, the iLet is capable of downloading software updates via a phone app and pushing it to the pump.
---------------------------------------------------------------------------------
The Algorithm
The iLet Bionic Pancreas uses an algorithm called Dosing Decision Software to deliver insulin. Unlike other commercially-available automated insulin delivery (AID) algorithms, Dosing Decision is an adaptive closed-loop system that uses super micro boluses (SMBs) to handle insulin delivery. In addition to not having a programmed background insulin delivery (basal insulin, aka basal rate or just basal), the iLet doesn't require exact carb counting for meals. Instead, you have to be "carb aware", which means you train the algorithm to your typical carb counts for each meal. I struggled with this and we'll talk about that in a second.
Dosing Decision is loosely based on the DIY loop algorithm, oref1. There are several significant differences between Dosing Decision and oref1, including the inability to set temporary blood glucose (bg) targets or adjust your target range, as well as adjust insulin action times. It's safe to assume these limitations are a concession to FDA approval. More aggressive (and recent) iterations of DIY looping algorithms include the ability to forego meal announcements entirely (this algorithm is known as dynamicISF).
Something to keep in mind when using the iLet: the algorithm does not work without a CGM, and there is no way to limp the pump along for more than 72 hours without one. After the initial training period (aka first 7 days of use) you can manually input bg values at set intervals to keep the pump running in "BG-run Mode" for up to 72 hours. If a low bg is entered, the iLet will shut off background insulin for an hour.
As a side note, the algorithm is aggressive in trying to prevent low bg (hypos), and you'll likely find that you need fewer carbs to treat a low bg. During pump training I was recommended 10g of carbs to start, and have found that 5-10g is typically plenty to bring me back into range.
---------------------------------------------------------------------------------
First Impressions: iLet Bionic Pancreas
My first impression of the iLet was that it's huge. It has a significantly bigger footprint (albeit lighter and slimmer) than the Tandem t:slim x2 and Medtronic Paradigm's that I used for decades. It's also very light, and the black and white, high contrast LCD touchscreen (boo touchscreens, but that's just me and my climber fingers struggling with them) can be read in bright sunlight and with polarized lenses, which is pretty great. There's a "button" at the top of the pump that you touch to bring up the unlock screen and turn on the backlight. It appears to be a pressure sensor of some variety, and I regularly hit it while the pump is moving around in my clothing or I'm fishing it out of a pocket or just holding it in my hand. Luckily, actually unlocking the pump requires deliberate (and often frustrating because I hate touchscreens) interaction.
It's worth noting that the primary reason the iLet is comparatively large is that the pump casing is set up to take two reservoirs, one for insulin and one for (eventually) glucagon-equivalent and act as a dual-hormone pump.
 |
| Left to Right: iLet, Tandem t:slim X2, Medtronic Paradigm (3.2mL), Paradigm (1.8mL) |
 |
| Left: iLet, Right: t:slim X2 |
 |
| Left: iLet, Right: Case |
---------------------------------------------------------------------------------
Getting Started
The initial algorithm training is short-lived (4-7 days or so) but I found it wildly stressful. The only input when you start the pump is your weight, so bg tends to run higher than normal for the first couple days until the algorithm has learned individual patterns. I had some issues with the algorithm horrifically under-estimating my insulin sensitivity in the evenings and driving my bg very, very low for hours. I actually had to announce a meal to get insulin on board in order to let my body actually use all the glucose in my bloodstream to, you know, fix the hypo. I had almost daily severe hypos during the first week on the iLet, and they were severe and lasted what felt like forever (but was really a couple hours). When I wasn't low, I was high, spending more time over 300 mg/dl in four days than I have in the past year.
It's worth noting that I am a bit of an unusual case as far as digestion and insulin sensitivity. Between the mild gastroperesis and extremely variable insulin sensitivity throughout the day, my ratios vary from 1u:25g to 1u:10g (carbs) and 1u:55 mgdl to 1u:35 mgdl (correction). Similarly, my basal rates historically range from 0.5u/hour to 1.6u/hour throughout the day. The point being, the entire premise of body weight to determine the starting point for the Dosing Decision algorithm was kind of a shit show for me.
Meal announcements are all relative to the "usual for me" meal, so if you generally eat 45g of carbs for dinner but sometimes it's 30g and sometimes it's 60g, it's appropriate to call all of the above "usual". The recommendation is to announce meals as "larger" if they're more than 1.5 times larger than your usual meal, and "smaller" if they're around half of your usual carbs. For small meals that are under 25% of a "usual" meal, don't announce it and let the algorithm handle it. As the algorithm gets trained, this works well and generally keeps bg below 180 mg/dl or knocks it back into range relatively quickly (and goes against 29 years of ingrained diabetes management techniques).
Being realistic with meal announcements can be hard, especially early on. If you find yourself calling a dinner "larger than usual" every few days, it's probably not actually larger and is more in line with your typical meal size. It turns out, I'm great at carb counting and lousy at recognizing what my typical carb intake is for different meals. The end result of this is I spent a lot of time trying to decide if a meal was less than, the same as, or more than my "usual" carb amount for aforementioned meal. I finally started calling the majority of meals "usual for me" and letting the algorithm handle the difference. This is unintuitive for me and feels like I'm courting disaster (even though it is definitely the appropriate way to do things). Note to self: most meals should, in fact, be "usual" when announced.
This brings us to the most difficult part of the iLet system for me (and probably other's who have been carb counting and micro-dosing insulin for years to get optimal results): being carb aware instead of carb counting.
During the initial algorithm training period (first 7 days or so), I failed horribly at bracketing my carb counts and tagged more meals as "larger" than I should have, which resulted in insufficient insulin delivery when I actually did eat larger meals. The algorithm updates itself regularly, but it takes time and you have to be consistent, which is not my strong suit. All that said, training the algorithm to update ISF (or in my case, correct user error during the initial period) only takes a couple days. This bodes very well for changes in insulin sensitivity due to hormones, illness, or other lifestyle changes.
Something to consider as far as meal announcements is that there is not a designated meal announcement for snacks. This is annoying for those of us who nibble throughout the day rather than eating regular meals. The iLet user manual recommends picking the approximate time of day and using the meal type associated with that for your announcement. If the snack has as many carbs as that typical meal, announce it using "less", "usual", or "more. If it's less than 25% of the carbs typical for that meal, don't announce it. This seems to work... usually. One workaround (suggested by the RN who trained me) is to designate one of the "less" meal announcements as a snack (assuming your snacks are 25-50% of the carbs typical of that meal). Since breakfast is not my meal of choice, I've tried using my "less " breakfast announcement for snacks, which seems to work okay, although I'm not convinced it's any better than using the "less" announcement for other meals. Rumor has it that there will be a Snack announcement added in an update, but who knows if/when that's actually coming.
The iLet Mobile App was updated in mid-2024 to mirror the pump screen, making it comparable in data viewing to the t:connect mobile app (at the time of original posting the app was very meh). It's easy enough to sync your pump to your phone and the app will automatically upload data from the pump when the app is open to the BetaBionics Cloud. Once data is synced, the Therapy Overview screen where you can view the data doesn't seem to work half the time and insists on claiming there is insufficient data (even if that is definitely not the case). When it does work, the data display is pretty nice. When looking at the insulin history, it helps to remember that the "basal" is the insulin being pushed unrelated to meal announcements to keep your bg in range.
---------------------------------------------------------------------------------
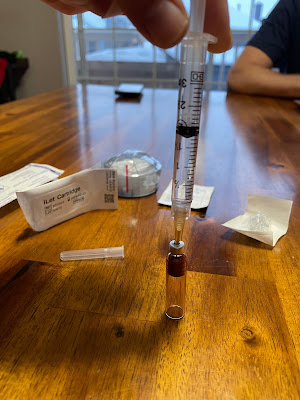
Getting going on the iLet was pretty straight-forward, all things considered (see above discussion on training the algorithm and the initial adjustment period as it learns). The most significant difference in day-to-day pump use has been changing the reservoir and infusion site. There's an additional part (the adapter between the reservoir and tubing) and the packaging is excessive, especially when you consider that Tandem has bundled their identical needle and syringe into one package.
The 180u reservoir has a functional maximum 160u after filling and priming. The plunger (red bit at the top of the reservoir shown below) doesn't have anything to prevent it from popping out, so you have to be careful not to overfill the res. You can (and probably should) mitigate this risk by setting the res on a hard surface while filling.
One of the super cool features of the iLet is the hella fast priming and insulin delivery. Like, super fast. Priming tubing during a site change takes literal seconds and I keep wasting insulin because I don't take my finger off fast enough. The iLet delivers insulin at a rate of 1u/3sec (20u/min). This is significantly faster than the standard delivery rate of the other commonly used insulin pumps (Medtronic, Tandem, and Omnipod have delivery rates of 1.5u/min, with a "fast" delivery rate of 15u/min available on some Medtronic systems). On the other hand, this means that big doses of insulin go in rapidly and if you're running an ultra-fast acting insulin like Fiasp or Lyumjev it can be spicy.
Speaking of priming, if you don't fill the reservoir all the way and need to "prime" more than 25u, the prime stops and you are prompted to confirm that droplets haven't appeared at the end of the infusion site. I find it a nice way that the pump helps keep you from getting distracted and wasting a bunch of insulin.

The pump auto-resumes insulin delivery after you fill a new cannula (if you select "yes") or complete the priming process (if you don't change your infusion set) with zero human intervention (compared to the t:slim which requires manual resuming, and the Medtronic pumps which don't resume delivery until you've backed out of the menu). Simply select the site type (teflon or steel) and cannula length, then hit go.
A couple things to note when it comes to site changes and alarms...
The pump gives an alert when an infusion site is 3 days old. There is no way to disable this. You can, however, accept the alert, let it navigate you to the site change menu, and then back out without going through any of the site change process. Boom. Problem solved.
The low reservoir alarm goes off at 20u (standard), and then again at 5u. Once you're at 5u remaining, every time the pump delivers insulin it's notifies you of the low reservoir. Annoying, yes, but quite useful if you're like me and run things aaaaaaaall the way down.
---------------------------------------------------------------------------------
Charging
The iLet can only be charged with a mag charger, which makes charging slow. The recommendation is to charge it 10-15 min a day, and I strongly suggest doing this (I've been charging it while I have my morning coffee). The battery drain isn't too bad, but seems to be 15-20% per day with a projected battery charge lasting 4-5 days. I haven't run it down past 60% because I don't want to sit around charging it for an eternity. On the other hand, you can charge the iLet using any high-quality mag charger (although they'll tell you that you must use the provided charging pad). Annoyingly, BetaBionics doesn't sell extra or replacement chargers, so you can't go buy a spare. Oh, and you have to remove the belt clip to place the pump on the charger. Dumb.
---------------------------------------------------------------------------------
I'm going to start off by saying that my biggest concern when starting the iLet was how it would handle exercise. I fully expected that I'd need to find new and creative ways to work around the algorithm given the wide variety and frequency of my physical activities. I am happy (and, frankly, shocked) to report that exercise is one place where the iLet Dosing Decision algorithm excels, and if we're being honest, is the only place I don't have complaints.
The recommendation from the iLet trainers is to disconnect during exercise if you think you may go low. This is stupid, especially for those of us who exercise for prolonged periods, be it hiking, long runs, or biking. The closest way to set a temporary bg target (like the higher bg target of Control IQ's Exercise Mode or Omnipod SmartAdjust's Activity feature) is to toggle on a Sleep schedule with a "higher" target bg. I've actually had fairly good success going into cardio pre-meals (aka fasting or at least 5 hours since last meal) and taking 10-15g of carbs 15-ish minutes before starting if my bg is trending down or sitting a bit lower than I'd prefer. This let's the food start kicking in (I'm not announcing it) about the time I start exercising so I combat potential hypos while side-stepping the algorithm delivering SMBs for the snack. If my bg trend is flat and above 90 mg/dl, I've been letting the algorithm do it's thing when I exercise.
I've done multiple fasted runs without disconnecting or taking any food on before starting with impressive results. Similarly, I haven't had any notable lows or highs after lifting weights (lifting often results in a bg spike, while running/cardio typically drops bg). There's no accounting for everything, so make sure to carry fast-acting carbs to treat any hypos during exercise.
My praise of the way the iLet handles exercise comes with one (massive) disclaimer: during the initial 3-7 days while the algorithm is training, do not try to exercise (especially cardio), as odds are good it will drive you into the ground and keep you there. Learn from my mistakes.
---------------------------------------------------------------------------------
A note on time in range
I considered putting this under "cons" but decided that wasn't fair to the algorithm or readers considering making a switch. Once the algorithm was trained, I've found myself running higher than I was using Control IQ and spending significantly more time sitting between 150 and 180 mg/dl. Recall that "in-range" for the Dosing Decision and CIQ algorithms is fixed at 70-180 mg/dl. This just so happens to be a larger range that what I prefer. The t:slim allows you to deliver manual boluses that I used to nudge my bg down to 100-120 mg/dl and prevent prolonged periods hanging out near the upper end of my range. Using the pump's target range of 70-180 mg/dl, my time in range for the past 14 days is 86% (compared to 91% on CIQ). However, my actual time in range for the past 14 days (70-160 mg/dl) is 78% on the iLet (compared to 85% for the most recent 14 days on CIQ). There's a moderate chance I'll see a slight increase in my A1C at my next doctor visit, but nothing that will be concerning from a medical outcome standpoint.
---------------------------------------------------------------------------------
- You can disable all CGM alerts on the pump except urgent low, which alarms at 55 mg/dl. This allows you to only have to interact with CGM alerts on one device (CIQ has alarms for out-of-CIQ-range that cannot be disabled). I wound up disabling all the CGM alerts on the pump and turning them on in the Dexcom app (you can also turn on alerts in a non-factory app like xDrip), since it's easier to access my phone than the pump. The only significant flaw with the CGM integration is that you can't adjust any of the alert thresholds on the iLet, so you either accept what they're fixed at or disable them and use a phone app for alerts.
- Speaking of CGMs, the bluetooth on the iLet is vastly superior to other pumps. I haven't lost connection with the CGM since starting the pump, and that includes a couple weeks using a very old transmitter (that then proceeded to expire). Unlike the t:slim, it doesn't seem to matter if the pump is facing in or out, or is on a different side of your body than the CGM, or if you lay on it while sleeping. From a user standpoint, this is a huge win.
- The infusion sites are identical to the Tandem equivalents listed on the BetaBionics website. Literally the same product (and factories, apparently) with a different label. This means that if you have extra Tandem supplies, you now have a bunch of extra iLet supplies. Yay!
Cons
- There is currently no ability to deliver meal announcements via the phone app, although this is apparently in the works. In this regard, Tandem has every other tubed pump on the market beat.
Since I'm complaining, I also have genuinely no idea what the purpose of the diagnostic download is when you sync the pump to the app - and I couldn't find any guidance regarding what it's supposed to do. The app does, however, check for any sideloaded applications or if the pump has been rooted or jailbroken and will block you from using the app if it determines you have done any after-market modifications. Interestingly, this insinuates that the pump can be relatively easily hacked and used for DIY looping.
- There is not currently a Suspend feature. If you're going to disconnect to shower or exercise, the suggestion is to put the pump far enough away that it's out of CGM range so it's not delivering micro-doses. Word on the street is that a suspend feature will be included in a software update (the trial version of the pump included one), so hopefully that won't be too long of a wait.
- There is no way to take a correction (or any manual) bolus. BetaBionics recommends you disconnect for 90 minutes if you take a correction with an insulin pen. Note that the correction algorithm is pretty aggressive, but it can still take 2-4 hours to get back in range. My experience has been that if you trust the loop the algorithm (especially with the "lower" bg target of 110 mg/dl) is good at knocking you back down while sticking the landing.
- I know I already said this, but the iLet Connect sticks out from the pump and catches on things. Like pockets and belts. If you're wearing womans pants with annoyingly small pockets, the pump barely fits, with the iLet Connect adding over half an inch to the length (it fits in pockets better without it, but that's not an option for actual operation of the pump).
Annoying
- IOB is only displayed under "algorithm steps" and not on the home/lock screen. Unlike some other commercial AID systems, the insulin on board (IOB) includes basal insulin, so the displayed value is higher than many of us would otherwise expect. This is because the algorithm pushes everything as SMBs rather than establishing a basal profile that it deviates from. Functionally, this is similar to how Medtronic's SmartGuard and Omnipod's SmartAdjust work with the bg and insulin delivery averaging over a series of days, and mimics several DIY loop algorithms.
- While you can adjust target bg (110 mg/dl = "lower", 120 mg/dl = "usual", 130 mg/dl = "higher), you can't customize the range - it's fixed at 70-180 mg/dl. There is not a way to set a temporary bg target, and if you want to run a bit higher for some reason, you have to go adjust your target value (or use a Sleep schedule and toggle it on/off as needed. I played around with this a bit and you can set a schedule that lasts for the full day so you don't have to mess around with times).
- The reservoir only holds 180u, making it not ideal for people with higher insulin needs or resistance.
---------------------------------------------------------------------------------
While there are several features of the iLet and the Dosing Decision algorithm that I don't love, the pump has some extremely good features. The use of SMB's by the algorithm has reduced the magnitude of my post-prandial spikes (no pump will eliminate them completely) and almost eliminated severe hypos. The hypo mitigation alone is a compelling reason to use the system. Convenience factors such as the black and white LCD screen that you can read in bright light and with polarized lenses and auto-resuming insulin delivery after a filling a cannula make interacting with the pump just a little bit easier. And don't forget the superiority of the bluetooth receiver that is able to maintain a basically continuous connection with the CGM, regardless of body placement.
Dosing Decision is the first loop algorithm (commercial or DIY) I've encountered that excels at aerobic and anaerobic exercise. The thing I was extremely skeptical of turns out to be the best part of the system for me, even going so far as to dramatically reduce bg drops during walks (and we all know that walks drop bg disproportionately). As much as trusting the loop can feel counter-intuitive when exercising, it really does shine if you let it do it's thing.
There are some features of the iLet and it's accessories that feel like lazy design, such as the large amount of packaging required for full site changes and the size of the iLet Connect that protrudes from the top of the pump.
Overall, I've found the iLet with Dosing Decision to be a mostly user-friendly device with an algorithm capable of adjusting to day-to-day variations in insulin needs. The interface for announcing meals and infusion set changes are intuitive, although some features (namely IOB and CGM and transmitter changing) are significantly less so. The iLet seems to be a system that reduces the mental burden of diabetes management, especially for people with diabetes who struggle with post-prandial spikes and accurate carb counting.
---------------------------------------------------------------------------------
Ultimately, I decided that I was happier using my Tandem t:slim x2 with CIQ over the iLet. Most of this was related to the ability to manually adjust doses and maintain a tighter bg range (this is very much an individual preference and not a judgement on the iLet's capabilities). I was more stressed out about my diabetes during the 3 months on the iLet than I'd been in years, which is a clear indication that it wasn't the right system for me.
I wound up testing out the BetaBionics 90-day return policy on day 89. To their credit, BetaBionics went to great lengths to make sure I was able to refund the pump and unopened and unused supplies. Their customer service team was top notch.
I firmly believe the iLet is a great system and would not discourage anyone from using it. Every AID system and algorithm is a little different and successful diabetes management is all about finding what works and is sustainable for you.